Special Populations in Geriatrics
These services can be provided at the ADRC, by telephone, or through a home visit, whichever is more convenient to you.
Services Provided by the ADRC
The ADRC can connect you to resources about:
- In-home personal care and nursing
- Housing options
- Housekeeping and chore services
- Home modifications
- Adaptive equipment
- Transportation
- Health, nutrition, and home-delivered meal programs
- Medicare, Medicaid, and Social Security
- Caregiver supports and respite
Dementia

The article below from the Mayo Clinic gives a great overview of dementia.
The article below provides information on how physical therapy services can help patients with dementia.
The staff at my final clinical rotation had the opportunity to go through the Virtual Dementia Tour. My CI said it gave him a much better understanding and greater empathy toward his patients with dementia as well as patients experiencing peripheral neuropathy, hearing and vision loss.
- In my first clinical at a SNF, the therapy staff were trained in the GEMS Brain change model. It breaks Dementia down into six stages and explains what the patient is going through in each stage. This helps promote understanding and empathy on the part of the caregiver toward the patient.

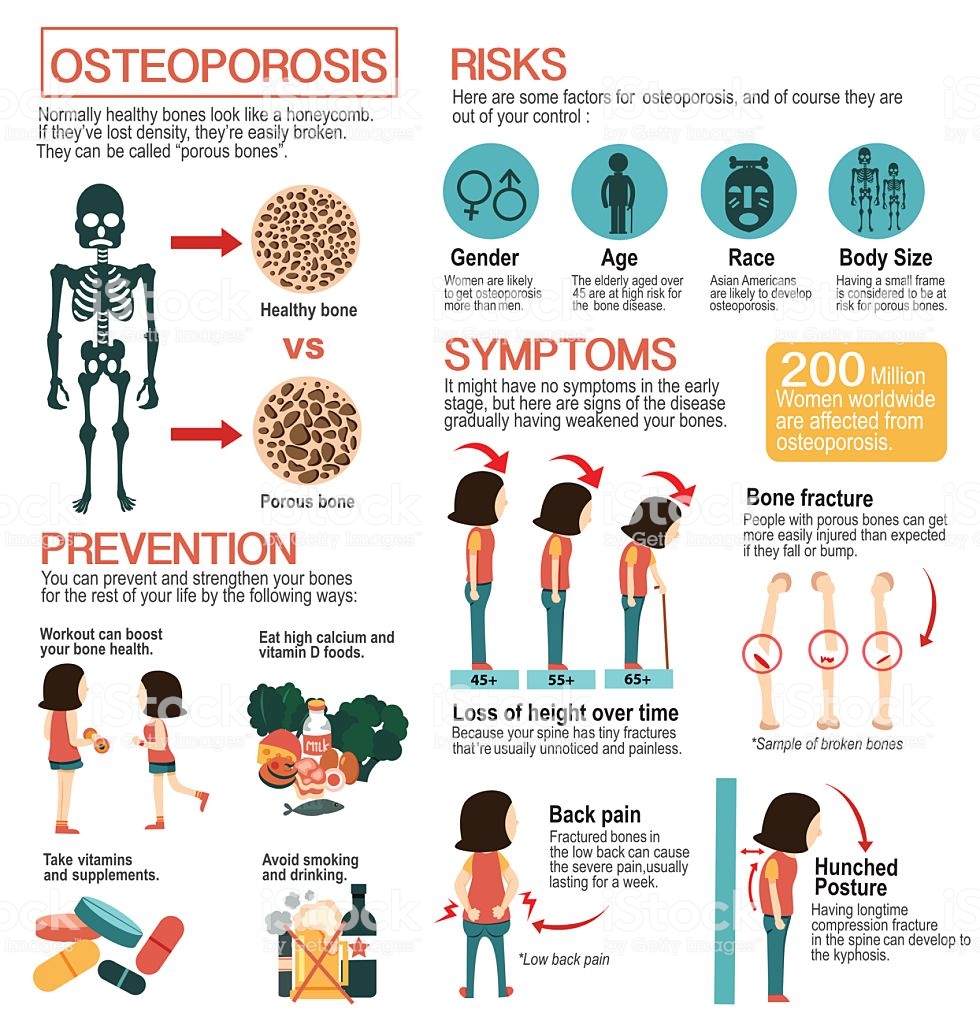
Osteoporosis
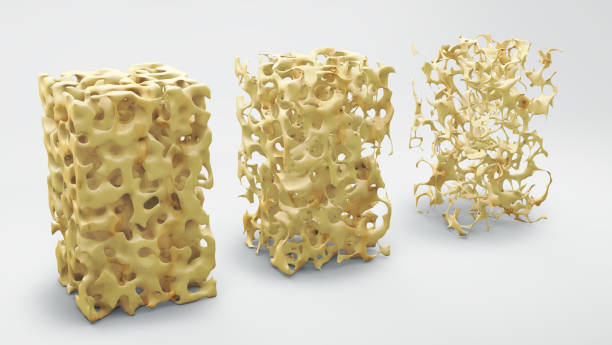
Osteoporosis is a metabolic bone disorder in which the rate of bone resorption speeds up while the rate of bone formation slows down. This leads to a reduction of bone mass which decreases bone density and strength. If affects about 10 million people in the U.S. and is the most common metabolic bone disease. There are several classification of primary osteoporosis including: idiopathic (both genders, all ages), involutional/senile (men and women over age 70) and postmenopausal (women 50-60 years old). Secondary osteoporosis is caused from a primary disease processes or as a side effect of certain medications (Giles, 2018, pg 536).
The loss of calcium and and phosphate salts, combined with the reduction of bone mass, causes brittle and porous bones that fracture easily. This is seen in both trabecular and cortical bone in the geriatric population and generally affects postmenopausal patients. All bones are affected but the most common locations of fractures include: vertebrae, distal radius/ulna and femoral neck (GIles, 2018, pg. 563).
Risk factors for primary osteoporosis:
- inadequate dietary calcium
- smoking
- excessive caffeine
- high intake of salt or alcohol
- small stature
- Caucasian race
- sedentary lifestyle
- family history or history of chronic disease
Secondary factors of osteoporosis:
- prolonged drug therapy of heparin or corticosteroids
- endocrine disorders
- malnutrition
- other disease processes
Patients may complain of low thoracic or lumbar pain, experience compression fractures of the vertebrae, and complain of back pain. Pain is acute and increases with weight bearing and palpation. Patients may also present with kyphosis, Dowager's hump, decreased height and other changes in posture (Giles, 2018, pg. 536). The best way to determine osteoporosis is with a bone density test, although Xrays can show the amount of degeneration and the reduction of bone density in a targeted area. Once osteoporosis progresses it can impact the scull, long bones and ribs. Spontaneous fractures and skeletal deformities are common and once a fracture occurs, the risk for subsequent fractures increases. Early detection and management is crucial in limiting long-term effects of the disease (Giles, 2018, pg. 537).
Physical therapy cannot cease the process of osteoporosis but it an empower the patient to manage the disease effectively. Patient education in the areas of exercises, positioning, pain management, nutrition, and fall prevention is necessary. Weight bearing exercises should be emphasized as tolerated. Some patients use a corset or lumbar support if they are at risk of vertebral fractures. Some patients need to be trained in the use of an assistive device. Aquatic therapy is a good option but should not replace weight bearing activities. Heavy resistive exercises, flexion exercises and ballistic movements should be avoided. The patient should be able to complete the prescribed exercise program independently (Giles, 2018, pg. 537).
Giles, S.M., (2018). PTA Exam, The Complete Study Guide. Scarborough, Maine: Scorebuilders.